28 year old male with cough and epigastric pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based inputs.
CHIEF COMPLAINTS
28 year old male came with the chief complaints of
cough since 5 days and
epigastric pain since 3 days
HOPI
Pt was apparently asymptomatic 5 days back then he had cough which was a dry type for 4 days and with sputum from today morning which is whitish in colour,non foul smelling, non blood stained . Fever for 1 day which is low grade and more at night relieved by taking medication.
Since 3 days he has epigastric pain which is insidious in onset gradually progressive aggravated in suline position and relieved by sitting and leaning forwards associated with giddiness
No H/ O burning micturition, hematuria
PAST HISTORY
N/K/C/O HTN , DM, TB, EPILEPSY, CAD, ASTHMA
DAILY ROUTINE
wakes up at 5:00 does his daily routines and goes to work ( in grampanchayath water department) And does not takes breakfast most of the days and takes lunch at 1: 00 pm and goes to work and returns home by 5: 00 and watches TV for some time and takes dinner by 9:00 pm and goes to bed by 10:00
FAMILY HISTORY
not significant
PERSONAL HISTORY
Diet - Mixed
Appetite- decreased
Bowel and bladder movements-passing urine regularly but did not pass stool for 2 days
Sleep-adequate
Habits-started consuming alcohol since 10 yrs initially occassionally but from 6 years started consuming daily ( 1 quarter)
GENERAL EXAMINATION
Patient is conscious coherent cooperative, well oriented to time place person
moderatly built and moderately nourished
Pallor- mild
icterus- absent
cyanosis- absent
clubbing- absent
Lymphadenopathy - absent
Edema- absent
VITALS
Bp - 100/70 mm hg
PR - 84 bpm
RR -20 cpm
GRBS - 130 mg/ dl
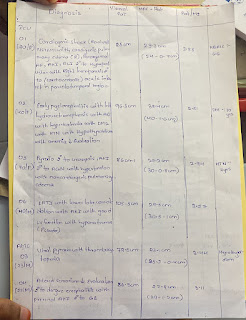
SYSTEMIC EXAMINATION
•CVS- S1, S2 heard
• RS- BAE present
• CNS - intact
•PA-
▪INSPECTION inspection- shape - schapoid and symmetrical
umbilicus- inverted and central in positionno visible scars, dilated veins
▪PALPATION- local rise of temperature in epigastric right hypochondriac, right lumbar, umbilicus area tenderness in epigastric and right hypochondrium ,
▪Hepatomegaly present, spleen not palpable
▪no palpable mass
▪Bowel sounds-heard
? Amoebic liver abscess
TREATMENT
1) INI MAGNEX FORTE 1.5 MG 1V/ BD
2)INJ TRAMADIL 1amp in 100 mk IV OD
3) INJ ZOFER 4 mg IV OD
4) INJ OPTINEURON 1 amp in 100 ml NS IV OD
5) IVF NS, RL @ 100 ml/hr















Comments
Post a Comment