I have been given the following cases to solve in an attempt to understand the topic of 'Patients clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations anddiagnosis and come up with treatment plan
This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to Medicine assignment based on comprehension of the cases
PULMONOLOGY CASE
55 year old female with shortness of breath, pedal edema and facial puffiness
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ans) Evolution of symptoms
• 1st episode of SOB :- 20 years ago (in month of january)
• Since then she had yearly episodes of SOB for 8 years lasting 1 week occurring around january
• 12 years ago another episode of SOB lasted for 20 days
•Then after yearly episodes for 12 years around january lasting for month SOB was (Grade- 2)
• Diagnosed with Diabetes 8 years ago
• Anemia and took iron injection:- 5 years ago
• Generalized weakness :- 1 month ago
• Diagnosed with Hypertension:- 20 days back
• Pedal edema:- since 15 days
•Facial puffiness:- 15 years back
LOCALISATION OF PROBLEM: Lungs
Primary etiology : could be due to pollen allergy or due to usage of chulha since 20 years
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient.
a)Head end elevation:-
• To reduce aspiration
• To improve oxygenation
• To reduce incidence of VAP
b)Intermittent BiPAP
• assist ventilation by producing positive expiratory amd inspiratory pressure
c)INJ AUGMENTIN
• To treat any infections caused by bacteria such as lower respiratory tract infections
d)TAB AZITHROMYCIN
• It is an antibiotic used to treat any infections of chest
e)INJ LASIX
• Used to reduce the edema
• Acts by blocking the absorption of sodium, chloride and water from filtered fluid in the kidney causes prof profound increase in the output of urine
f)INJ HYDROCORTISONE
• improve lung function
g) NEB with IPRAVENT and BUDECORT
• it may ease intake of drugs
h) TAB Pulmoclear
• it is bronchodilator and mucolytic
• Relieve the congestion and blockage
3)What could be the cause of her acute exacerbation
May be due to INFECTION( infection causes inflammation in lungs leading to narrowing of airways , blockage may occurs due to swelling and mucus production
4)Could the ATT have affected her symptoms ?If so how?
May or may not be ( few studies shown hepatotoxicity occurred within 15 days of treatment if that was the case it leads to liver damage and hypoproteinemia and causes edema)
5)What could be the cause for her electrolyte imbalance?
May be due to RIGHT HEART FAILURE ( Decreased cardiac output leads directly to reduction renal blood flow , with impairment of renal exceretion of water and ELECTROLYTES
NEUROLOGY CASES
CASE :1
A 40 year old male with complaints of IRRELEVANT TALKING and DECREASED FOOD INTAKE
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
•Diagnosed type -2 diabetes 2 years back
•2 TO 3 episodes of seizures 1 year ago
•4 months ago recent episode of seizures with restlessness ,sweating,tremors
Irrelevant talking and decreased food intake since 9 days
▪LOCALISATION OF LESION :- could be brain
▪PRIMARY ETIOLOGY: may be due to ALCOHOL WITHDRAWALmay due to Thiamine deficiency results in WERNICKE ENCEPHALOPATHY
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient
a)Thiamine INJ : To reduce alcohol enceohalopathy and as a supplement to cope with thiamine deficiency
b)LORAZEPAM : acts by stimulating GABA- A receptors , during the withdrawal of one agent the other may act substitute
prevents agitation, alcohol withdrawal seizures delirium, tremors
c)PREGABALIN : reduce synaptic release of several neurotransmitters
reduces withdrawal symptoms
d)LACTULOSE: Reduces the intestinal absorption and production of ammonia
use in preventing and treating portal- systemic encephalopathy
e)POT CHLOR and INJ KCL : used to supplement the potassium
3)Why neurological symptoms appeared this time, that were absent during with drawl earlier ? what could be a possible cause for this time?
Actually there were neurological symptoms during previous with drawl (GTCS , restlessness , sweating and tremors), now also it is because of alcohol with drawl
When you drink , the alcohol suppress certain neurotransmitters in the brain
When neurotransmitters are no longer suppressed , but are used to working harder to overcome the suppression they go into a state of over excitement . If you suddenly stop drinking or significantly reduced the amount the it can cause alcohol withdrawal.
ALCOHOL WITHDRAWAL TIMELINE
•Stage 1 : 6 to 12 hours after last drink (anxiety , insomnia ,LOSS OF APPETITE , etc)
•Stage 2 : 12 to 24 hours after last drink (tactile hallucinations ,auditory hallucination,VISUAL HALLUCINATIONS)
• Stage 3: 24 to 48 hours after last drink (WITHDRAWAL SEIZURES ) • Stage 4: 48 to 72 hours after last drink
or may due to Thiamine deficiency results in WERNICKE ENCEPHALOPATHY
4) What is the reason for giving Thiamine in this patient?
Thiamine is prescribed to prevent wernicke encephalopathy a acute disorder due ti thiamine deficiency manifested by confusion, ataxia, opthalmoplegia and korasakoff syndrome, which is manifested by memory impairment and amnesia.
THIAMINE DEFICIENCY IN ALCOHOL ABUSERS RESULTS FROM
- In-adequate dietary intake.
- Reduced gastro intestinal absorption on consumption of alcohol.
- Decrease hepatic storage.
- Im-paired utilisation.
5) What is the probable reason for Kidney injury in this Patient?
Kidney has an important job of filtering harmful substance . Alcohol is one among them.
- Kidney's of heavy drinkers have to work harder.
- Alcohol causes change in the function of Kidney and make them less able to filter the blood.
- It also affects the ability to regulate fluid and electrolyte in body
- By promoting liver disease, chronic drinking adds to Kidney's job and the rate of blood flow to Kidney is usually kept at certain level so that Kidney can filter the blood well. (Established liver disease impair this balancing act)
- Drying affect of Alcohol effects the normal function of cells and organs including Kidney.
- Due to free radicals (produced due to break down products of Alcohol) which intern triggers tissue injury and increased inflammationj.
In addition alcohol can disrupt hormones that effect Kidney function.
6) What is the probable cause of Normocytic anemia?
History showing decreased food intake which may lead to malnutrition leading to reduction of nutrients and prevents the production of new red blood cells and may be due to decreased production of erythropoeitin from damaged Kidney.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If Yes, how and Why?
If the cause of ulcer is due to diabetes, it occurs due to decreased flow of blood (Ischemia) and due to peripheral neuropathy (no damage) that may be aggravated by alcohol toxicity because of poor nutrition leading to poor wound healing and problems with nerves. And in chronic alcoholism, immune system is weak which may lead to decreased wound healing.
CASE:2
A 52 year old male with Cerebellar Ataxia.
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient's problem?
7 days back : Giddiness associated with one episode of vomiting
Then asymptomatic for 3 days he consumed a small amount of alcohol
Then he developed : giddiness associated with aural fullness ,bilateral hearing loss,tinnitus,2 to 3 episodes of vomiting's
DENOVO hypertension
LOCALISATION OF LESION: Presence of Infract in the Inferior Cerebellar hemisphere of the Brain
PRIMARY ETIOLOGY: Ataxia is the loss of muscle control or coordination of Voluntary movements such as, Walking or Picking up of objects.
In this case, Patient is a known case of denovo hypertension. For this he has not taken medication.
Stroke is due to infract can be caused by blockage or bleeding in the brain, due to which brain is deprevied of Nutrients and Oxygen. This may lead to infract formation.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient
a)VERTIN TAB: It is an anti histamine, as the patient is suffering from bi-lateral hearing loss, aural-fullness, tinnitus (Simulating meinieres disease)
It acts as a agonist on H1 receptors
b)ZOFER: Ondensetron to treat nausea and vomiting
▪ acts antagonist of 5H3 receptors on vagal afferents in gut and even block receptors in CTZ and solitary tractus nucleus
c)Tab ECOSPRIN : aspirin it is anti platelet reduces the platelet adhesiveness and aggregation and there by preventing clot formation
d)Tab ATORVOSTATIN: acts as a HMG Co A reductase inhibitor rate limiting step in cholesterol biosynthesis thus decreasing blood LDL and VLDL
used for primary prevention of stroke
e)CLOPIDOGREL: it is antiplatelet drug thereby preventing clot formation
f)THIAMINE: as the patient is alcoholic there may be chance of Wernickes encephalopathy
so to prevent it thiamine is given
g)Tab : MVT : it is methylcobalamine given in case of vitamin B12 deficiency
3) Did the patient's history of denova hypertension contribute to this current condition?
Cerebellar infract is usually caused by blood clot obstructing blood flow to Cerebellum.
High blood pressure is a risk factor for the formation of Cerebellar infracts.
Increased shear stress caused on blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelal dis-function in this case. Hign BP can also promote cerebral small vessel disease. All these factors contribute to the stroke.
4) Does the patient's history if Alcoholism make him more susceptible to Ischaemic or Haemorrhagic stroke?
Light to Moderate consumption of Alcohol lower's the risk of Ischaemic stroke but it had no impact on the risk of developing Haemorrhagic stroke.
Alcohol consumption lowers the level of fibrinogen, a protein helps in formation of clot. So, there by decreases chance if Ischaemic stroke.
However heavy alcohol consumption increases the chance of Haemorrhagic stroke.
Heavy drinker's have 1.6 times more chance of intra cerebral Haemorrhage and 1.8 times increased chance subaracnoid Haemorrhage.
However heavy alcohol intake is associated with impaired fibrinolysis, increased platelet activation and increased BP & Heart rate. So, in this case, history of alcoholism coupled with his hyper-tension could be a cause of stroke.
CAES -3
45 year old female with palpitations pedal edema radiating pain along the left upper limb
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient's problem?
• Episode of bilateral upper and lower limb paralysis ten years back
• Right and left Paresis due to hypokalemia 2 months back
• Bilateral pedal edema since 8 months
• Infection 7 months back
• Pain radiating along left hand associated with tingling and numbness since 6 days
• Chest pain and difficulty in breathing since 5 days
▪ PRIMARY ETILOLOGY :- may be due to hypokalemia causing the palpitations, chest heaviness and generalised weakness
Radiating pain along her left upper limb due to cervical spondylosis
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
May be due to usage of diuretics
other risk factors
• Inadequateintake:anorexia,dementia, total parental nutrition
• abnormal losses due to medications :diuretics corticosteroids enema laxatives
Real causes: osmotic dialysis, corticoid excess, Renal tubular acidosis
Transcellular shift :alkalosis ,thyrotoxicosis, delirium tremans,current hypokalameic periodic paralysis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
• Earliest changes: decreased T wave amplitude, ST depression ,T wave inversion or flat, prolonged PR interval, presence of u waves
• symptoms of hypokalemia: weakness and fatigue palpitations, muscle cramps and pains, anxiety, psychosis ,depression delirium
CASE-4
A 55 year old male patient with altered sensorium and involuntary movements
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
▪ Cells in the brain sends electrical signals to one another the electrical signals passes along nerves to all the parts of the body .A sudden abnormal burst in electrical activity causes disurption of signals to nerves leading to seizures
▪ Having stroke increases the risk of having a seizure stroke causes brain become injured. Injury to brain causes in scar formation which effects electrical activity .Disruption of electrical activity can result in seizures.
▪ People with hemorrhagic shock are are more likely to you have stroke than those with the the ischemic stroke
▪ Increased risk of seizures if stroke is severe or occurs within the cerebral cortex of brain .
▪ 2018 study showed 9.3 percentage of all people with stroke experience a seizures
▪ Seizures following ischemic stroke
Could be due to hypoxia, metabolic dysfunction, hypoperfusion, increase in intracellular calcium sodium with a resultant lower threshold for depolarization,etc these all are postulated as neurological etiologies
▪ Seizurs following haemorrhagic stroke
Could be due to irritation caused by products of blood metabolism or hemosiderin deposits are also thought to be cause irritability after a hemorrhagic stroke
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Abnormal increasing in in activity of frontoparietal Association cortex related subcortical structures is associated with loss of consciousness in generalised seizures. Abnormal decreased activity in same networks may cause loss of consciousness in complex seizures
Diverse seizures types including absence ,generalised tonic clonic and complex partial seizures converge on the same set anatomical structures through different mechanisms to disrupt conciousness
CASE-5
A 48 year old male with seizurse and altered sensorium
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
As patient is a chronic alcoholic - Damage from alcohol is common cause of cerebellar ataxia. It can also cause associated science of peripheral neuropathy.
Inside the brain, alcohol directly damages cetail cell within cerebellum and rest of brain, and those people who drink excessively over a period of time, it can cause particularly severe and often permanent damage.
Peripheral neuropathy is a damage to body peripheral nervous system. This can cause muscle weakness, numbness and tingling burning pain, and loss of co-ordination. This peripheral neuropathy can contribute to the ataxia.
Once damage has occurred, ataxia symptoms continues to progress if you continue to drink excessive amount of alcohol.
and also the patient had a history of minor head injuries
2) What was the reason for his IC Bleed? Thus alcoholism contribute to bleeding diatheses?
Chronic alcoholism associated with hypertension may predisposed to ICH. But, in our patient there is no hyper tension. So, probable cause would be "Impaired coagulation mechanism" (In alcoholics with hepatic damage, there could be decreased concentration of clotting factors resulting in increased fibrinolysis. This could have known if LFT was done and CBP was done for Platelet count for this patient.
CASE-6
A 30 year old male patient with weakness of right upper limb and lower limb.
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
1.Does the patient's history of road traffic accident have any role in his present condition?
Yes, this might be the cause as the history shows dislocationof zygomatic mandibualr process, there could be a chance of injury to cranium and causes injury to small blood vessels and it resulted in present condition
2.What are warning signs of CVA?
• Problems with movement or walking
• Trouble speaking and understanding
• Dizziness or problems with balance or coordination
• Weakness and numbness of face arms or legs usually on one side of body
• Severe headache with no known cause especially if they happen suddenly
3.What is the drug rationale in CVA?
•For ischaemic stroke
a) Emergency IV medication includes IV injection of Recombinant tissue plasminogen Activator(tpc) is also called as ALTEPLASE it is a gold standard treatment for schumak stroke this drug dissolves blood clot and improves blood flow
b)ECOSPIRIN
• it decreases the production of prostaglandins and thrombaxane .Its ability to suppress the produciton is due to irreversible inactivation of COX enzyme
• It mainly reduce inflammation ,analgesic , Prevents formation of clots, reduces fever
c)ATORVASTATIN
▪it is a statin acts by competitively inhibitng HMGCOa reductase and there by preventing conversion of HMGCoA to
mevalonate and there by decreasing cholesterol production in liver
▪ it is given to prevent the heart disease including heart attack and stroke
d)MANNITOL
Mannitol by its osmotic effect reduce the cerebral edema .It may improve cerebral perfusion by decreasing viscosity , and as free radical scavanger it might act as neuroprotecatant
e) RT feed: to provide nutrition to those
people who does not ontain nutrition through mouth or not in a state of swallowing food
•For haemorraghic stroke
▪Emergency treatment of haemorrhagic
Stroke : If blood thinners are given to prevent clots we must give drugs or blood transfusion to counteract the effect of blood thinners and drugs to to reduce intracranial pressure ,to prevent spasm of blood vessels and to prevent seizures
▪ Surgical procedures should be done
4. Does alcohol has any role in his attack
? Mild alcohol drinking has a protective role in in Ischeamic stroke and no effect on hemorrhagic stroke, but heavy alcohol drinking have impact on hemorrhagic stroke. As the patient is occasional alcohol drinker this may not play the role for present attack, as patient has history of accident and minor head injuries this these may be the cause present attack
But alcohol may or may not have affected the the healing process of those minor injuries as patient is occasoinal drinker
5.Does his lipid profile has any role for his attack??
In lipid profile we are seeing there is slight decrease in HDL level there is there will be inverse relation between serum HDL cholesterol and occurrence of stroke so there might be chance of occurrence of stroke in this patient
CASE-7
A 50 year old patient with cervical myelopathy
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
1)What is myelopathy hand ?
▪It is a characteristic dysfunction of hand been observed in in various cervical spine injuries and cervical myelopathy when there is involvement of spinal cord
▪There is is loss of power off adduction and extension of ulnarr two and three fingers and inability to grip and release rapidly with this fingers. This change has been observed as Myelopathy hand and it it appears due to tract Pyramidal tract involvement
Myelopathy hand sign shown on right side
2)What is finger escape ?
•" wartenberg sign" is a a neurological sign consisting of involuntary abduction of 5th (little finger) caused by unopposed action of extensor digital minimi
•This finding of weak finger adduction in cervical myelopathy is called as finger escape sign
• this is one of the the sign to elicit myelopathy hand
3)What is Hoffman’s reflex?
▪Name from a German scientist John Hoffman
▪It examines a persons reflex and is used to examine the reflexes of upper extremities
▪ this test is a a quick way to test for possible existence of spinal cord compression from a lesion of spinal cord or or another underlying conditions
CASE-8
A 17 year old female with seizures
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1.
1) What can be the cause of her condition ?
maybe due to cortical vein thrombosis with hemorrhagic venous infarction involving right posterior temporal lobe
2) What are the risk factors for cortical vein thrombosis?
▪Infection: meningitis, otitis media, mastoiditis
▪Drugs: oral contraceptives ,steroids, inhibitors of angiogenesis
▪Chemotherapy: cyclosporine and l- asparginase
▪Prothrombotic state :Pregnancy ,peurperium, antithrombin deficiency, protein c and protein S deficiency ,hormone replacement therapy
▪ Mechanical :head trauma, lumbar puncture
▪Inflammatory: sarcoidosis, inflammatory bowel disease, SLE
▪ Malignancy
▪Dehydration
▪ Nephrotic syndrome
▪ Intracranial :Dural fistula ,Venus anomalies
▪ Vasculitis: Bachets disease, wegener's granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Seizures are resolved and seizures free period got achieved even after medical intervention but sudden episode of seizure was maybe due to persistence of existing foci by abnormal firing of neurons
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Presence of risk factors should should raise suspicion of cortical venous sinus thrombosis.
Anticoagulants are used for the prevention of harmful blood clots CLEXANE(enoxaparin)low molecular weight heparin binds and potentiate antithrombin 3 ,protease inhibitor to form complex and Irreversible inactivates factor Xa
CARDIOLOGY CASES
Case 1
78 year old male with shortness of breath chest pain bilateral pedal edema and facial puffiness
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Heart failure is a complex clinical syndrome arising from deficient cardiac output that is unable to meet the the metabolic needs of the the organ and tissues in the body
Ejection fraction to to percentage of blood left ventricle the heart main pumping chamber that is pumped out each time the ventricle contracts this is most often measured with echocardiogram
▪ Heart failure with preserved ejection fraction(HFrEF)
•also referred to as "diastolic heart failure" the heart muscle contract normally but the ventricle do not relax as they should during ventricular filling (or when the ventricle relax)
• it is preceded by chronic comorbidities such as hypertension type 2 Diabetes mellitus obesity and renal insufficiency
▪ Biological process
Cell adhesion
Leukocyte migration
Inflammatory response Neutrophil degranulation
Integrin mediated signalling Pathways
Extracellular matrix organisation
▪ specific markers
integrin subunit beta 2
Catenin beta 1
▪ Heart failure with reduced ejection fraction(HFrEF)
• Also referred to as "systolic heart failure".Left ventricle loses its ability to contract normally
•it is often preceded by the acute ok chronic loss of cardiomyocytes due to you ishceiam,a genetic mutation, myocarditis or valvular disease
▪ Biological processes Regulation of sequence specific DNA binding transcription Smooth muscle cell proliferation
Nitric oxide biosynthesis
▪ Specific markers
AMP dependent transcription factor activation N terminal Pro b type natriuretic peptide
Growth differentiation factor 15
Interleukin 1 receptor
2.Why haven't we done pericardiocenetis in this pateint?
• Pericardiocentesis is a procedure is is done to remove fluid that has built up in the sac around the heart
• Pericardiocentesis is not done here because the effusion was self healing it reduced from 2.4 cm to 1.9 cm
3.What are the risk factors for development of heart failure in the patient?
• high blood pressure
• smoking
• diabetes
• alcohol abuse increases the risk of atrial fibrillation, heart attack and congestive heart failure
• diabetes
• AV block can be associated with severe bradycardia and hemodynamic instability it has a greater risk of progressing to third degree heart block ( complete)or astysole
• worsening of pericardial effusion leading to cardiac tamponade
4.What could be the cause for hypotension in this patient?
Visceral pericardium maybe thickened which is restricting the the heart to expand causing hypotension
CASE-2
73 year old male patient with pedal edema shortness of breath and decreased urine output
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-
pedal.html
1.What are the possible causes for heart failure in this patient?
Patient has diabetes since 30yrs and also having diabetic related neuropathy-retinopathy - nephropathy, so there is an increased risk for heart failure
* Hypertension since 19yrs - important risk factor
* Chronic alcoholic since 40yrs, leads to decreased LVEF and causes LV dysfunction
* patient has elevated creatinine, chronic kidney disease, AST/ALT greater than 2,all of this are important risk factors for heart failure
2.what is the reason for anaemia in this case?
•As a patient is a chronic alcoholic so etiology of anaemia chronic alcoholics is complex and multifactorial causes could include poor nutrition liver dysfunction and ineffective erythropoiesis
• Alcohol can be directly toxic 2 bone marrow as suggested by free erythroblast vacuolation or sideroblastic changes alcoholism and the debilitating factors with which it is often associated example chronic sepsis and poor nutrition frequently causes market anemia enough liver diseases is absent
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
As patient is chronic alcoholic and also diabetic both of them may contribute for non healing ulcer
As diabetics causes decrease blood flow (ischemia)and due to peripheral neuropathy this may cause ulceration
This may be aggravated by alcohol toxicity because of poornutrition leading wound healing and problem with nerves
4. What sequence of stages of diabetes has been noted in this patient?
There are 4 stages in type 2 diabetes insulin resistence ,prediabetes ,type 2 diabetes and vascular complications including retinopathy nephropathy neuropathy and or related micro vascular events
The patient is diagnosed with diabetic triopathy exhibiting sequence of neuropathy retinopathy and nephropathy
The patient has been diagnosed with diabetic retinopathy CKD stage 4 and shows signs of diabetic neuropathy such as numbness
CASE-3
A 52 year old male with A-fib and bilateral thrombus
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?▪10yrs ago - Operation for Hernia ▪Since 2-3 yrs - Facial puffiness
▪1 yr ago - SOB grade II
▪1 yr ago - was diagnosed with Hypertension.
▪Since 2 days - SOB which progressed from Grade II to Grade IV.
▪Since 2 days - Decreased urine output
▪.Since 1 day - Anuria
ANATOMIC LOCALISATION: Atria ( SA node)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
a)DIGOXIN
It is a cardiac glycoside act by increasing intracellular sodium that will cause influx of calcium and and there by increasing Contraction
used for heart failure and arrhythmia
b)CARVEDIOL
It is a beta blocker, and thereby lowers heart rate and blood pressure
Used for Hypertension heart failure LV dysfunction with MI
c)HEPARIN
It is an anti-coagulant , acts by inactivating thrombin and activated factor X through an antithrombin dependent mechanism
Used for Prophylaxis and treatment of venous thromboembolism and pulmonary embolism; Atrial fibrillation with embolization ; chronic consumptive coagulopathies.
d)ACITROM
It is an Oral anti-coagulant.This prevents carboxylation of Vitamin K dependent clotting factors, II, VII, IX, X and interferes with coagulation.
Used for Thromboembolic diseases as DVT, Coronary occlusion
e)CARDIVAS
It is an adrenergic blocker.Reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevent a response to the sympathetic nervous system, leading to decreased Heart rate and contractility
used for Hypertension, Angina and heart failure.
f)DYTOR
It is a diuretic .Antogonizing effect of Aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
Used for Edema, Hypertension.
g) Pan d
It is a Proton pump inhibitor
Used for Heavy bloating, gas, heart burn, indigestion, GERD.
h)TAIMX
It is a cephalosporin antibiotic
UUsed forTreatment of infections of throat, airway and urinary tract ; Typhoid fever.
I)THIAMINE
For Wernicke's encephalopathy, infantile beriberi etc.
j)Inj HAI
It is a short acting insulin.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
•Cardiorenal syndrome, a complex pathophysiological disorder of both the heart and kidneys, is a condition in which acute or chronic damage to one organ can lead to acute or chronic dysfunction of the other organ
•Physiological, biochemical and hormonal disturbances as parts of the main pathogenic mechanisms of cardiorenal syndrome
Depending on primary organ dysfunction and disease duration, there are five different types of cardiorenal syndrome. Type 1 cardiorenal syndrome (acute cardiorenal syndrome) is defined as acute kidney injury caused by sudden decrease in heart function. Type 2 cardiorenal syndrome (chronic cardiorenal syndrome) refers to chronic kidney disease linked to chronic heart failure. Type 3 cardiorenal syndrome (acute renocardial syndrome) is caused by acute kidney injury that leads to heart failure. Type 4 cardiorenal syndrome (chronic renocardial syndrome) includes chronic heart failure due to chronic kidney disease. Type 5 cardiorenal syndrome (secondary cardiorenal syndrome) is reversible or irreversible condition marked by simultaneous heart and kidney insufficiency, as a result of multiorgan disease such as sepsis, diabetes mellitus, sarcoidosis, amyloidosis, etc Now the patient has CARDIO RENAL SYNDROME 4
4) What are the risk factors for atherosclerosis in this patient?
The risk factors for atherosclerosis are hypertension, high cholesterol and triglyceride, DM-1, obesity, physical inactivity, smoking, high saturated fat diet.
This patient has Hypertension, physical inactivity and obesity
5) Why was the patient asked to get those APTT, INR tests for review?
The patient was on Anticoagulants. So to predict the occurrence of CVA and ischemic attacks, the patient is advised to get these tests.
CASE-4
https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
67 year old patient with acute coronary syndrome
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
• 12 yrs ago - Diagnosed with DM 2 •Since 1yr - Heartburn which is relieved with medication •7months ago - Diagnosed with Pulmonary TB, she completed the ATT course. •6 months ago - Diagnosed with HTN
•Since half hour - Severe SOB even at rest
ANATOMICAL LOCALISATION:CVS
ETIOLOGY:may be due to atherosclerosis due to the presence of diabetes
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
a)MetXL
It is a Beta-blocker and slow down heart rate, and makes pumping more efficient.
Used for Hypertension, Angina, arrhythmias, migraine.
b)TELMA
It is an Angiotensin receptor blocker.
It binds to angiotensin II type 1 receptors with high affinity, causing inhibition of action of Angiotensin II on vascular smooth muscle leading to reduction in arterial blood pressure.
Used for HTN, diabetic nephropathy, CHF
c)GLIMI
Glimepiride + Metformin
The primary mechanism of action of Glimepiride is stimulating release of insulin from functioning pancreatic beta cells. Metformin reduces insulin resistance.
Indications - DM 2
3) What are the indications and contraindications for PCI?
▪Indications for PCI
•Acute ST-elevation myocardial infarction (STEMI)
•Non–ST-elevation acute coronary syndrome (NSTE-ACS)
•Unstable angina.
•Stable angina.
•Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
•High risk stress test findings.
▪Contraindications for PCI
•Lack of cardiac surgical support.
•Critical left main coronary stenosis without collateral flow from a native vessel or previous bypass graft to the left anterior descending artery.
•Coagulopathy.
•Hypercoagulable states.
•Diffusely diseased vessels without focal stenoses.
4)What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
Every procedure has its indications to perform,and the complications associated with those procedures ,Its the duty of doctor to do the procedures when and where required ,and we need to keep the financial status of the patient procedure so the complications with this procedure could be Bleeding ,Blood vessel damage,Allergic reavtion to dye Arrhythmias,Need for coronary artery bypass grafting. Because of these complications it is better to avoid the proceducre in those who does not need
▪OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
•Research on overtesting and overtreatment is important as they are more harmful than useful.
•Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Overdiagnosis through overtesting can psychologically harm the patient.
Hospitalizations[41] for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systemsThe use of expensive technologies and machineries are causing burden on health care systems
.
CASE-5
A 60year old Male patient with chest pain,giddiness
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?•Since 8 yrs - DM 2
•Known case of HTN
•5 days ago - received COVISHIELD vaccination
•Since 3 days - Chest pain
•Since morning - Giddiness and Sweating
ANATOMICAL LOCALISATION:Blood vessels
PRIMARY ETIOLOGY:Myocardial infarction is usually due to occlusion of the coronary vessel caused by rupture of a vulnerable plaque.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
a)ASPIRIN -
•It is an NSAID.
• It inhibits COX-1 and COX-2 to decrease the Prostaglandin and thromboxane synthesis.
• They are used as anti platelet drugs to prevent clot formation and stroke.
b)ATORVASTATIN
• It is a statin.
• It is a HMG CoA reductase inhibitor and thus inhibits the cholesterol synthesis. It decreases VLDL, LDL in the blood, cholesterol synthesis. It increases LDL receptors in the liver and increases LDL uptake and degeneration. Thus decreasing LDL levels in the plasma.
• Used as Primary hyperlipidemias and prevention of stroke.
c)CLOPIDOGREL
• Antiplatlet medication
• It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
• Used to and prevent stroke and heart disease
d)INJ HAI
It is a short acting insulin
e)ANGIOPLASTY
Angioplasty also known as balloon angioplasty and percutaneous transluminal angioplasty is a minimally invasive endovascular procedure used to widen narrow or obstructed arteries or veinstypically to treat arterial atherosclerosis.
.3. Did the secondary PCTA do any good to the patient or it was unnecessary?
. The secondary PCI was not necessary in this patient.
Ideally PCI should be done within 12 hrs of onset of symptoms
•PCI performed from 3 to 28 days after MI it does not decrease the incidence of death reinfarction or New York heart association (NYHA)classIV heart failure
• But it is associated with higher rates of both procedure related And true STelevation reinfarction.
•LatePCI leads to the increased risk of periprocedural complications long term bleeding and stent thrombosis.
CASE-6
87 clear year old male patient with shortness of breath constipation decreased urine output
https://kattekolasathwik.blogspot.com/2021/05/a-case-of-cardiogenic-shock.html
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
•Fluid might have increased the heart's pumping ability
.As Cardiogenic shock is a life-threatening condition in which your heart suddenly can't pump enough blood to meet your body's needs. so fluids might have improved hearts pumping activity by incresing
•So fluids might have increased the cardiac output and applied supplied required systemic oxygen demand and there by reduced shortness of breath
2. What is the rationale of using torsemide in this patient
As the patient has from abdominal distension it might be due to Ascites Aas there is underlying heart problem
Aaj torsemide is a diuretic it treat edema (fluid retention; excess fluid held in body tissues)
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
As the patient has dribbling of urine with oliguria and a previous history of TURP they might have suspected UTI and empirically ceftriaxone was given.
GASTROENTEROLOGY (AND PULMONOLOGY) Cases
Case-1
A 33 YEAR OLD MAN WITH PANCREATITIS, PSEUDOCYST AND LEFT BRONCHO-PLEURAL FISTULA
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
•1st episode of pain abdomen and vomiting :5 YEARS BACK
•Stopped taking alcohol for 3 years
•1 year back 5 to 6 episodes of pain abdomen and vomiting after starting to drink alcohol again
•20 days back increased consumption of toddy
•Since 1 week pain abdomen and vomiting
•Fever constipation and burning micturition :since 4 days
▪ANATOMICAL LOCALISATION: Pancreas
▪PRIMARY ETIOLOGY:ALCOHOL INTAKE,CHRONIC and LARGE AMOUNTS,and also his addictions of taking KHAINI and GHUTKA
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
a)Amikacin, Metronidazole andMeropenam:
•They are given to control infection.
b)TPN : Total Parenteral Nutrition:
• It is given to bed ridden patients,it contains carbohydrates ,proteins, fats vitamins and minerals
c)NS/RL:
• It is given as fluid replacement in order to combat dehydration
d)Tab. Pantop:
• It is a proton pump inhibitor.it is used in this case for its anti pancreatic secretory
e)Inj.Octreotide:
•It is a somatostatin analogue
•It decreases the secretions of pancreas
•It also has anti inflammatory effects
f)Inj.Thiamine:
•It is Vitamin B1 supplement.
•It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
•Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
g)Inj.TRAMADOL:
It is an opioid analgesic which is given to relieve pain.
▪MY APPROACH:
MAY BE SAME AS THE ABOVE PHYSICIANS AND I WILL SUGGEST TO CONSULT A PSYCHIATRIST FOR DEADDICTION COURSE ONCE HE BECAME NORMAL
Case-2
25 YEAR OLD MALE WITH EPIGASTRIC PAIN
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
•Dyspnoea is due to some inflammation in lungs- PLEURAL EFFUSION
•with the severe pancreatitis there are a lot of inflammatory chemicals that are secreted into the blood stream. These chemicals create inflammation throughout the body, including the lungs. As a result, a person may experience an inflammatory type of reaction in the lungs called ARDS.
2) Name possible reasons why the patient has developed a state of hyperglycemia?▪Acute Pancreatitis causes damage to pancreatic cells and it will leads to relative hypoinsulinemia and hyperglucagonemia
▪May be due to edema of pancreatic tissues and
▪Inbitory effect of trypsin on insulin production
▪Hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress or the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
•As patient is an ALCOHOLIC ,,there might be liver injury,so the liver enzymes got elevated,
•Coming to SPECIAL MARKERS of Alcoholic Liver Disease,serum GGT,AST,ALT,MCV,etc; are being in run ,
•But a ratio of AST:ALT more than 2,highly of suggestive of alcoholic liver disease.
4) What is the line of treatment in this patient?
The main course of treatment for acute pancreatitis is to maintain electrolyte balance and to maintain volume status. (IVF)
- INJ.TRAMADOL: for relief of pain
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v as an anti emetic
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
Case-3
A 45 year old female patient with fever, pain abdomen ,decreased urine output and abdominal distension
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
1) What is the most probable diagnosis in this patient?
MAY BE THE ABDOMINAL HEMORRAGE
.This will give rise to abdominal distension and blood which is aspirated
▪D/d
•Ruptured liver abscess
•secondary hemorrage or fluid collection may be due to hollow viscous perforation
•intraperitoneal hematoma
•Grade 3 Renal parenchymal disease
2) What was the cause of her death?
After leaving the hospital patient underwent laparotomy at another Hospital. The next day patient died. This may be due to complications of laparotomy hemorrhage infection or or damage to internal organs
3) Does her NSAID abuse have something to do with her condition? How?
Yes I think so,some of the researches available in google and some literature says that NSAIDS ABUSE can lead to several problems :
•gastrointestinal ulcers, bleeding
•nephrotoxicity(acute kidney injury)
•bronchospasm
•cardiovascular problems,etc;
Source:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4809680/
NEPHROLOGY (AND UROLOGY) CASES
Case-1
52 year old male patient with shortness of breath burning micturition and fever
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
1. What could be the reason for his SOB ?
It may be due to ACIDOSIS caused by Renal failure because of Hydronephroureterosis
2. Why does he have intermittent episodes of drowsiness ?
might be due to Electrolyte imbalance(Hyponatremia)
3. Why did he complaint of fleshy mass like passage in his urine?
▪They might be the necrosised tissue of kidney and may be pus cells resulted from inflammation due to obstructive nephropathy and hydronephrosis and the necrosised material might have appear to him as fleshy mass
Source:https://www.hindawi.com/journals/ijn/2020/8846622/
▪Acute tubular necrosis(seen as granular muddy casts as fleshy masse in urine) due to obstructive nephropathy
Source:https://en.wikipedia.org/wiki/Acute_tubular_necrosis
4. What are the complications of TURP that he may have had?
Possible complications in this patient include:
- Electolyte abnormalities
- Pain during micturition
- UTI
- Urinary bladder thickening
Case-2
An eight year old with frequent urination
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
1.Why is the child excessively hyperactive without much of social etiquettes ?
•As of now,exact reason cannot be said, but it might beADHD(Attention Deficit Hyperactive Disorder),in this case the child is hyperactive,impulsive,does not have proper social etiquettes as is expected of his age, too active to pay any attention at school, talk so fast that even comprehending sentences becomes quite difficult.
•children will be in developing stage,various type of influences can affect children mentalstatei.eparents,family,relatives,friends,residency,environment,etc;
spending some more time wqith the child may give the same diagnosis or it might be overlapped with similar disorder.
•Some of the symptoms seen in ADHD are:
- They wont listen properly when we directly talk to them
- nonstop talking1
- avoid school,homework
- excessive anxiety,etc;
2. Why doesn't the child have the excessive urge of urination at night time ?
As he is sleeping at that time ,provocative stimuli will be absent ,and he will less anxious,at that time.
3. How would you want to manage the patient to relieve him of his symptoms?
•Although the cell counts in the urine examination, and there are no microorganisms after urine culture , still due to the presence of some mildly enlarged mesenteric lymph nodes, there still remains suspicion of an infective etiology, including cox bacilli.so we can prescribe antibiotics •To prevent abnormal involuntary detrusor
muscle contraction occuring in the wall of bladder we give- Anticholinergics
•To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
•Stimulants such as Methylphenidate,heAmptamine can be used
INFECTIOUS DISEASE (HI VIRUS,MYCOBACTERIA,GASTROENTEROLOGY,PULMONOLOGY) CASES:
Case-1
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
CLINICAL FINDINGS
She has difficulty in swallowing since 2 months,for both solids and liquids,and getting cough after taking food or water,the cough initially is a non productive and later associated with sputum,
She gets fever episodes since 2 months,she got weightloss and SOB and vomiting episodes,
PHYSICAL FINDINGS:
Laryngeal crepitus: positive (aspiration?or tracheooesophageal fistula?)
R.S - wheeze present in bilateral mammary areas.
Thinly built and moderately nourished.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
•A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome (IRIS)
•Whether elicited by an infectious or noninfectious agent, the presence of an antigenic stimulus for development of the syndrome appears necessary. This antigenic stimulus can be intact, “clinically silent” organisms or dead or dying organisms and their residual antigens.
Diagnostic Criteria for IRIS
Major criteria
▪Atypical presentation of “opportunistic infections (OI) or tumors” in patients responding to antiretroviral therapy.
▪Decrease in plasma HIV RNA level by at least 1 log10copies/mL.
Minor criteria
▪Increased blood CD4+ T-cell count after HAART
▪Increase in immune response specific to the relevant pathogen, e.g. DTH response to mycobacterial antigens.
▪Spontaneous resolution of disease without specific antimicrobial therapy or tumor chemotherapy with continuation of antiretroviral therapy.
Cohort analyses examining all manifestations of IRIS estimate that 17–23% of patients initiating ART will develop the syndrome.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221202/
PREVENTION OF IRIS:
▪Complications of IRIS can be prevented by careful monitoring the patients with low CD4+ cell count and a thorough history of co-infections. Clinicians should be aware of the fact that in spite of the initial restoration of CD4+ counts the patient has high chances to develop IRIS in a course of time.
▪Given that severe CD4+ T cell deficiency when ART is commenced is a risk factor for an IRIS, prevention of CD4+ T cell depletion through early diagnosis and treatment of HIV infection regardless of CD4+ T cell count, as supported by the findings of the START study (33), is the most effective measure for reducing the risk of developing an IRIS Inclusion of maraviroc in the ART regimen of patients commencing ART with a CD4+ T cell count of <100/μL was explored as a means of preventing an IRIS in the CADIRIS study (47) but was ineffective. Prednisolone therapy during the first 4 weeks of ART decreases the risk of TB-IRIS in HIV patients with CD4+ T cell counts <100/mL \
Source: https://hivmanagement.ashm.org.au/immune-reconstitution-inflammatory-syndrome-and-other-immune-reconstitution-disorders/prevention-of-an-iris/
INFECTIOUS DISEASE AND HEPATOLOGY CASES:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?
▪ Amoebic liver abcess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
▪ It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
2.What could be the cause in this patient ?
The consumption of locally made alcohol like toddy,saara,etc; could be the cause of his liver abscess.
SOURCE:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
Yes, the most common area affected with liver abscess is RIGHT LOBE as it got more blood supply.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
large liver abscess which is going to rupture
large anscess which is >/ 5 cms
left lobe abcsess
anscess which failed to resolve with medicine,etc;.
Case-2
1. Cause of liver abcess in this patient ?
The patient is taking toddy which might got contaminated with entamoeba histolytica and it might lead to liver abscess formation.
2) How do you approach this patient ?
In hematology reports,increased leucocyte counts are seen ,indicating infection and inflammation.
In biochemical tests(LFT) ,liver enzymes are elevated.
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
•We gave medicines for both amoebis cause and bacterial cause,the medicines given are:
•INJECTION. ZOSTUM 1.5 gm IV BD (twice daily) (Sulbactam+Cefaperazone):as anti-bacterial medicine.
•INJECTION. METROGYL 500mg IV TID ( thrice daily ):as anti-amoebic medicine
•TAB. DOLO 650 mg SOS (if needed)
•TAB. ULTRACET 1/2 QID( four times a day)
• INJECTION. OPTINEURIN 1amp in 100 ml •NS( Normal Saline) IV OD ( once daily)(Multi Vitamin)
•As the medicine given are working effectively, and patient got relieved from symptoms, so there is no need for aspiration and aspiration itself got some other coomplications.
4) Is there a way to confirm the definitive diagnosis in this patient?
We can confirm by ultrasonography and serological examinations.
INFECTIOUSDISEASES(MUCORMYCOSIS,OPTHALMOLOGY,OTORHINOLARYNGOLOGY,NEUROLOGY)
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
.3 years ago- diagnosed with hypertension
•21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
•18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
•11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
•4 days ago- patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lowerlimbs
In the evening patient periorbital oedema progressed
serous discharge from the left eye that was blood tinged
was diagnosed with diabetes mellitus
patient was referred to a government general hospital
•patient died 2 days ago
▪ANATOMICAL LOCALISATION:
NASAL CAVITIES ,PARA NASAL SINUSES , ORBIT
▪ETIOLOGY:
Mucormycosis is a life threatening infection that occurs in severely immunocompromised patients, while in diabetic ketoacidosis ,the immune system is compromised and the fungal spores entered through nasal cavities,eyes and through food or water, makes the patient vulnerable and causes rhinocerebral mucormycosis.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
The treatment will be consisting of :
1)INJ. LIPOSOMAL AMPHOTERICIN B
2)ITRACONAZOLE TAB will be given and dosage will be according to his creatinine clearance.
For Diabetic Ketoacidosis:
3)Fluid replacement
4)Electrolyte replacement
5)INSULIN THERAPY
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
According to me,
Increased use of steroids for lond durations and large doses in covid patients.
In INDIA type 2 diabetes mellitus is an epidemic and in these patients getting covid-19 and usage of unregulated steroid usage that too in large doses and for long time will lead to mucormycosis.
one point to be noted is as INDIA is a tropical country black fungus aka mucormycosis spores will be presenty in all conditions and in all environments
For more information,you can know by the link below:
QUESTION 9
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe
3) Indicate for each patient, the day of Covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe Covid (for example, altered sensorium, hypotension etc).
I have compiled all the data collected in the form of an excel spreadsheet, so as to be able to draw a comparative analysis about the progression of disease and the outcome in various patients.
https://aitharaveena.blogspot.com/2021/06/covid-cases.html
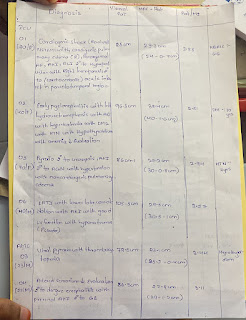
MASTER CHART
https://drive.google.com/file/d/1-5L742ps4ysQzmZTUdLF8nAKE4tTNFht/view?usp=sharing
MEDICAL EDUCATION
As a final year student where clinicals are important it is made possible even in lockdown through this online platform this process I came to know about the cases in hospital while sitting at home.Through this patient based online learning .I came to know about different topics related patients diseases and handmade me to search about them using various literature researchers and resources around the world





































Comments
Post a Comment