16 yr old male with
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based inputs.
CHIEF COMPLAINTS
16 year old male patient came with chief complaints of
•fever since 7 days
HOPI
Pt was apparently asymptomatic 7 days then he had fever which is high grade associated with chills and rigors more during night times. relieved by medications if taken every 4 hrly.
4 episodes of vomitings 4 days back with food as content non projectile non blood stained
There are 4 episodes of loose stools 3 days back after consuming papaya leaf juice and relieved by medication
NO H/ O cold, cough, headache, body weakness, burning micturition, hematuria, epigastric pain
PAST HISTORY
N/K/C/O ASTHMA , EPILEPSY
FAMILY HISTORY
His grand mother has dm and htn since 17 years
DAILY ROUTINE
studying inter 1st year waked up.at 6: 30 does his daily routines and takes breakfast at 7:30 goes to clg at 9: 00 pm and takes lunch at 1:00 college ends at 4:00 he goes to home by 4: 30 goes to stadium and plays there and does his home works and takes dinner at 7: 30 and uses mobile for 10 to 15 mins before going to bed . and sleep by 9: 30 pm
PERSONAL HISTORY
Diet - Mixed
Appetite- normal
Bowel and bladder movements- Regular
Sleep-adequate
Addictions- no
GENERAL EXAMINATION
Patient is conscious coherent cooperative, well oriented to time place person
moderatly built and moderately nourished
Pallor- absent
icterus- absent
cyanosis- absent
clubbing- absent
Lymphadenopathy - absent
Edema- absent
VITALS
Pt is c/c/c
Temp-
BP- 120/80 mm hg
PR- 55 bpm
RR- 18 cpm
SYSTEMIC EXAMINATION
CVS- S1, S2 heard
RS- BAE+
CNS- intact
PA- Soft , non tender
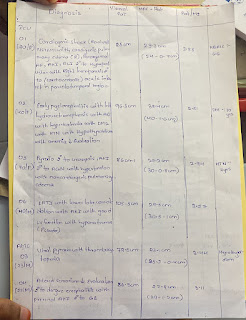
INVESTIGATIONS
DAY-1


















Comments
Post a Comment