32 year old male patient with Fever, giddiness, vomiting
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of
CASE
32 year old male patient came to opd on 20th of august with chief complaints of
▪ FEVER since morning
▪ Giddiness and vomitings since afternoon
HISTORY OF PRESENTING ILLNESS
Patient was apparantly asymptomatic 4 days back then he had abrasion on the right leg on 16th for which he had not taken any first aid following which he was asymptomatic for 4 days then he developed
▪Fever associated with chills on 20th and which was high grade not associated with cold, cough, head ache, shortness of breath and no diurnal variations is seen ▪Pain in the right calf which was dragging in nature radiating to thigh so that patient was not able to walk aggravating on walking and movement of leg and relieved on rest and medication
For which patient went to rmp where he was given IV fluids following which he had
▪ Vomiting 1st episode which was non billious, non projectile, and food contents are present not associated with epigastric pain , constipation and loose motions
after going home he had Giddiness rotational, not associated with headache ,sweating, palpitations, blurring of vision, diplopia, evening and 2nd episode of vomiting and went to rmp then he referred to present hospital
▪ On presentation:- cold extremities present , Pulse- feeble, BP:- 70/40 started on fluid resuscitation
He was kept in ICU and was shifted to general ward on 27th august and patient now complaints of only pain on movement of leg
PAST HISTORY
Patient had asthma since childhood , exacerbates on exposure to cold and on medication for it
Not a known case of diabetes, hypertension, epilepsy, tuberculosis, any chronic illness
PERSONAL HISTORY
Diet:- mixed
Appetite:- normal
Bowel and bladder movements:- regular
Sleep:- adequate
Addictions:-
• Alcohol- 4 times a day 1/2 quarter to 1 bottle since 20 years
•Kaini- daily since 5 years
• smoking :- occasionally since 20 years
▪No known allergies
FAMILY HISTORY
not significant
GENERAL EXAMINATION
•Patient is conscious ,coherent, cooperative , well oriented to time , place ,person
▪Moderately built and moderately nourished
Pallor:- absent
Icterus:- absent
Cyanosis:- absent
Clubbing :- absent
Lymphadenopathy:- absent
Edema:- absent
VITALS
At admission:- (20/08/2021)
Temperature:- 99.4 F
Pulse rate:- 60 bpm( low volume)
Respiratory rate:- 12cpm
BP :- 70/40 mm of hg
Spo2:- 97% at room temp
GRBS:- 96mg%
BP:- 130/90 mm hg
PR:-95 bpm
GRBS:- 98mg/dl
25/08/2021
Temperature:- 98.6F
BP:- 130/90mm hg
PR:- 65 bpm
26/08/2021
PR:- 64bpm
BP:- 120/90mm of hg
GRBS:-122mg/dl
27/08/2021
PR:-65bpm
BP:-130/80mm hg
28/09/2021
PR:- 72bpm
BP:-120/90mm of hg
▪CVS- S1 ,S2 hears no added murmurs and thrills
▪Respiratory system:- Normal vesicular breath sounds audible
▪ Abdomen:-obese, tenderness elicited in epigastric hypochondrial region, no palpable mass
▪ Cns:- Intact
INVESTIGATIONS
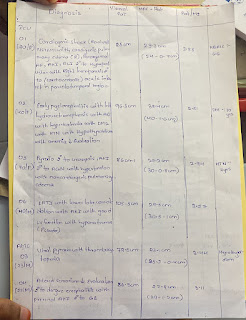
HEMOGRAM
ECG
ULTRASOUND REPORT
Septic shock secondary to right leg cellulitis
TREATMENT REGIMEN
20/08/2021
IVF- NS,RL- 200ml/kg/ hr-------10ml/kg/hr
Inj- ceftriaxone 1gmIV/ BD
Inj- Pantop-80mg mgIV 100 ml NS IV/ stat
Inj-Thiamine 300 mg IV 100ml NS IV/ stat
Inj- ondonsetron 4mg IV / stat
Inj - tramdol 1 AMP 100 ml NS IV/TID
BP,PR -2nd hrly nmiotoring
TEMP charting- 4th hrly
I/O - charting
21/08/2021
IV fluids- RL, DNS,NS@200mg/ hr
Inj- ceftriaxone-1gm IV/BD
Inj-PANTOP- 40 mg IV/OD
Inj- Zofer 4mg Iv/sos
Inj - tramdol 1 AMP 100 ml NS IV/BD
Inj- optineuron 1 amp M 100 ml NS IV/OD
Strict I/O charting
BP,PR,TEMP,SPO2- charting
Inj- noradrenaline 20 amp in 46 ml NS
(increase or decrease according to MAP 60-70)
Inj- metrogyl 100 ml Iv/Tid
22/08/2021
IV fluids- RL, DNS,NS@200mg/ hr
Inj- ceftriaxone-1gm IV/BD
Inj-PANTOP- 40 mg IV/OD
Inj- Zofer 4mg Iv/sos
Inj - tramdol 1 AMP 100 ml NS IV/BD
Inj- optineuron 1 amp M 100 ml NS IV/OD
Strict I/O charting
BP,PR,TEMP,SPO2- charting
Inj- noradrenaline 20 amp in 46 ml NS
(increase or decrease according to MAP 60-70)
Inj- metrogyl 100 ml Iv/Tid
23/08/2021
IV fluids- RL, DNS,NS@200mg/ hr
Inj- ceftriaxone-1gm IV/BD
INJ metrogyl 100 ml iv/ TID
INJ Pan 40 mg iv/ bd
Inj zofer 4mg iv/ Tid
Inj optineuron 1 amp in 100 ml NS Iv / oD
TAB pcm 650 mg TID
Tab chymoral forte Tid
Inj tramadol 1 amp in 100ml NS IV
Temp chartnig and tepid sponging 4th hrly
Stirct I/O charting
Bp, PR, RR, temp ,spo2 monitoring
24/08/2021
IV fluids- RL, DNS,NS@200mg/ hr
Inj- ceftriaxone-1gm IV/BD
INJ metrogyl 100 ml iv/ TID
INJ Pan 40 mg iv/ bd
Inj zofer 4mg iv/ Tid
Inj optineuron 1 amp in 100 ml NS Iv / oD
TAB pcm 650 mg TID
Tab chymoral forte Tid
Inj tramadol 1 amp in 100ml NS IV
Temp chartnig and tepid sponging 4th hrly
Stirct I/O charting
Bp, PR, RR, temp ,spo2 monitoring
25/08/2021
IV fluid with optineuron@ 100 ml/ hr
Inj ceftriaxone 1gm IV /BD
Inj metrogyl 100 ml Iv/TID
Inj pan 40 mg IV / OD
TAB Pcm 650 mg TID
Tab chymoral forte TID
strict I/O charting
BP. PR ,TEMP , spo2 monotoring
Tab ultracet QID( 1/2-1/2-1/2-1/2)
26/08/2021
IV fluid with optineuron@ 100 ml/ hr
Inj ceftriaxone 1gm IV /BD
Inj metrogyl 100 ml Iv/TID
Inj pan 40 mg IV / OD
TAB Pcm 650 mg TID
Tab chymoral forte TID
Bp,PR ,TEMP , spo2 monotoring
Tab ultracet QID( 1/2-1/2-1/2-1/2)
27/08/2021
IV fluid with optineuron@ 100 ml/ hr
Inj ceftriaxone 1gm IV /BD
Inj metrogyl 100 ml Iv/TID
Inj pan 40 mg IV / OD
TAB Pcm 650 mg TID
Tab chymoral forte TID
Bp,PR ,TEMP , spo2 monotoring
Tab ultracet QID( 1/2-1/2-1/2-1/2)
28/08/2021
IV fluid with optineuron@ 100 ml/ hr
Inj pan 40 mg IV / OD
TAB Pcm 650 mg TID
Tab chymoral forte TID
Bp,PR ,TEMP , spo2 monotoring
Tab ultracet QID( 1/2-1/2-1/2-1/2)










Comments
Post a Comment