50 YR OLD FEMALE WITH FEVER AND MALAISE
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case...
CASE
A 50 year old female came to OPD on 5th of may with chief complaints of
▪ FEVER since 5 days
▪ MALAISE since 5 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 5 days back and she developed fever and malaise
Fever was continuous type and relieves on taking medication , not associated with chills and rigors no diurnal variations,no complaints of vomitings ,chest pain, loss of smell loss of taste,shortness of breath
Patient got tested on 5th of may for Covid-19 and was positive
Patient got discharged on 7th of may
Patient presented to hospital on 8th may with SHORTNESS OF BREATH(GRADE 3) and LOW OXYGEN SATURATION (fluctuating between 86-92% on RA)
• Diabetes is detected in this admission
Patient got discharged on 19/05/2021
HISTORY OF PAST ILLNESSk
Not a known case of hypertension , asthma epilepsy, tuberculosis,any chronic illness
PERSONAL HISTORY
Diet ; Mixed
Appetite: Normal
Sleep:Adequate
Bowel and bladder movements :Regular
No addictions
No known allergies
FAMILY HISTORY
No significant family history
No other family member tested positive for covid 19
GENERAL EXAMINATION Patient is conscious, coherent and cooperative , well oriented to time place and person
She is moderately built and moderately nourished
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing:absent
Lymphadenopathy; absent
Edema: absent
VITALS
On the day of admission ( 08/05/2021)
Temperature: 98 F
Pulse rate : 101 per min
Respiratory rate ; 20 cycles/min
Blood pressure; 110/70 mm of hg
SPO2 ; 99%on 10 litres O2
GRBS; 56 mg%
09/05/2021
Pulse rate; 84 per min
Blood pressure: 110/70 mm of hg
SPO2; 99% with 10 litres of O2
GRBS; 56mg%
10/05/2021
Pulse rate; 80 per min
Blood pressure ; 110/70 mm of hg
SPO2 : 99% with 10 litres of O2
GRBS; 326mg/dl
11/05/2021
Pulse rate : 80 per min
Blood pressure : 110/70 mmg of hg
Respiratory rate ; 24 cycles per min
SPO2 : 98% with 10 litres of O2
Temperature ; 97.4 F
12/05/2021
Temperature ; 97 F
Pulse rate ; 80 per min
Blood pressure ; 110/70 mm of hg
SPO2 : 95% with 10 litres of O2
GRBS : 236 mg/dl@ 8am
377mg/dl@ 1pm
286mg/dl@8pm
13/05/2021
Pulse rate ; 94 per min
Blood pressure ; 120/60 mm of hg
SPO2 : 99% with 10 litres of O2
GRBS: 310mg/dl@ 8am
375mg /dl@ 1pm
238mg/dl@8pm
14/05/2021
Pulse rate:78 per min
Blood pressure:110/70mm of hg
SPO2: 97% with 10 litres of O2
GRBS: 238mg/dl @ 8am
15/05/2021
Pulse rate : 80 per min
Blood pressure: 110/70 mmof hg
SPO2 : 88% on 15 litres of O2
Temperature : afebrile
16/05/2021
Pulse rate:86 per min
Blood pressure: 120/80 mmof hg
SPO2: 90%
Temperature : 98.4F
GRBS: 248mg/dl
17/05/2021
Pulse rate ;84 per min
Blood pressure:120/60mm of hg
SPO2 :96% with 5 litres of O2
Temperature:afebrile
18/05/2021
Pulse rate:86 per min
Blood pressure :110/70 mm of hg
SPO2: 95% on 2 litres of O2 On the day of discharge( 19/05/2021)
Temperature: afebrile
Pulse rate:84 per min
Blood pressure :110/70 mm of hg
SPO2:95% with 2 litres of O2
SYSTEMIC EXAMINATION. . CVS: S1 and S2 heard no added thrills and murmur. .RESPIRATORY SYSTEM:Normal vesicular breath sounds audible
Dyspnoea: Grade 3
.ABDOMEN: Soft ,No tenderness, No hepatomegaly, No spleenomegaly
CNS: Intact
INVESTIGATIONS
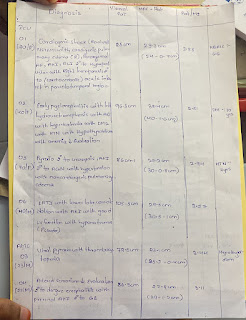
COMPLETE BLOOD PICTURE
09/05/2021:
Haemoglobin: 14.5gm/dl
Total count :7500cells/cumm
Neutrophils:83%
Lymphocytes:14%
Eosinophils ;01%
Monocytes: 02%
Basophils:0%
Platelet count: 2.01lakhs/cumm
Smear :Normocytic normochromic
11/05/2021
Haemoglobin: 13.2gm/dl
Total count :8100cells/cumm
Neutrophils:88%
Lymphocytes:07%
Eosinophils:02%
Monocytes:03%
Basophils:0%
Platelet count: 1.79 lakhs/cumm
Smear: Normocytic normochromic with relative Neutrophilia
16/05/2021
Haemoglobin:`12.2gm/dl
Total count:8600cells/cumm
Neutrophils:73%
Lymphocytes:19%
Eosinophils:04%
Monocytes :04%;
Basophils:0%
Platelet count:2.98 lakhs/cumm
Smear:Normocytic normochromic
RENAL FUNCTION TEST
Urea:60mg/dl
Creatinine:0.8 mg/dl
Uric acid:5.2 mg/dl
Calcium:9.6mg/dl
Phosphorous:3.6mg/dl
Sodium:130mEq/L
Pottasium: 4.4mEq/L
Chloride:95mEq/L
LIVER FUNCTION TEST
Total bilurubin:0.66mg/dl
Direct bilurubin:0.18mg/dl
SGOT( AST):21IU/L
SGPT(ALT):14IU/L
Total proteins:6.0gm/dl
Albumin:3.3gm/,dl
A/G RATIO:1.20
SERUM ELECTROLYTES
Sodium: 130 mEq/L
Potassium: 4.5 mEq/L
Chloride: 94 mEq/L
ARTERIAL BLOOD GAS ANALYSIS
PH: 7.35
Pco2 :23.0
Po2: 118
HCO3 :12.6
St.HCO3: 16.2
BEB: -10.7
BEecf: -11.9
TCO2: 24.2
O2 stat: 96.3
O2 count: 22.4
COMPLETE URINE EXAMINATION
Colour:Pale yellow
Appearance: Clear
Reaction: Acidic
Sp Gravity: 1.010
Albumin: +
Sugar:+++
Bile salts:Nil
Bile pigments:Nil
Pus cells: 3-6
Epithelial cells:2-4
Red blood cells:Nil
Crystals: Nil
Casts:Nil
Amorphous deposits:Absent
Others:Nil
POST LUNCH BLOOD SUGAR
604mg/dl ( on 9/5/2021)
SARS COV-2 QUALITATIVE PCR
POSITIVE
ECG REPORT
TRP GRAPH REPORT
D DIMER
970ng/ml
PROVISIONAL DIAGNOSIS
VIRAL PNEUMONIA SECOmNDARY TO COVID 19, TYPE 2 DIABETES MELLITUS
TREATMENT REGIMEN
ON THE DAY OF ADMISSION (08/05/2021)
O2 inhalation to maintain SpO2 >92%
T Dolo 650mg sos/po
BP,PR,Spo2 monitoring,
Inj. Pan 4o mg OD
09-05-2021
O2 inhalation to maintain SpO2 > 92%
Tab: Dolo 650 mg/sos/po
BP, PR, SpO2 monitoring
GRBS monitoring 6th hourly
Insulin Actrapid
NS/100 ml per hour
Duolin/ Budecort/Nebulization 8th hourly
Inj: PAN 40mg IV/OD
10-05-2021
Head end elevation
O2 suplementation- If SpO2 < 95%
Tab: Dolo 650 mg/po/sos
Tab: Pantop 40mg/po/BBF (8am - x - x )
Tab: Limcee/po/OD ( x - 2pm - x )
Nebulization/Duolin & BUDECORT 8th hourly
IVF: NS @100ml per hour
Inj: Insulin Actrapid 6ml per hour infusion
GRBS charting hourly
Monitor vitals
11-05-2021
Head end elevation
O2 suplementation- If SpO2 < 95%
Tab: Dolo 650 mg/po/sos
Tab: Pantop 40mg/po
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
IVF: NS @100ml per hour
Inj: Insulin Actrapid 6ml per hour infusion
Inj: Oseltamavir 75mg BD
Inj: CLEXANE 40mg s/o OD
Syp: CREMAFFIN PLUS (10 ml - 10 ml)
BP, PR,SpO2 monitoring
GRBS monitoring second hourly
12-05-2021
Head end elevation
O2 suplementation- If SpO2 < 95%
Tab: Dolo 650 mg/po/sos
Tab: Pantop 40mg/po
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
IVF: 2ONS @75ml per hour
Inj: HAT 6ml per hour in fusion
Inj: Oseltamavir 75mg BD
Inj: CLEXANE 40mg s/c
Syp: CREMAFFIN PLUS (10 ml - 10ml)
BP, PR,SpO2 monitoring
GRBS monitoring second hourly
13-05-2021
Head end elevation
O2 inhalation to maintain- If SpO2>90%
Tab: Dolo 650 mg/po/sos
Tab: Pantop 40mg/po/OD
Tab: Limcee/po/O Nebulization/Duolin & BUDECORT 8th hourly
IVF: 2ONS @75ml per hour
Inj: HAT 6ml per hour in fusion
Inj: Oseltamavir 75mg BD
Inj: CLEXANE 40mg s/c o/d
Syp: CREMAFFIN PLUS (10 ml - 10 ml)
BP, PR,SpO2 monitoring
Betadine mouth gargles- dilution with water
GRBS monitoring second hourly
14/05/2021
Head end elevatio. O2 inhalation to maintain- If SpO2 > 90%
Tab: Dolo 650 mg/po/sos
Tab: MUT OD
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
IVF: 2ONS @75ml per hour
Inj: HAT 6ml 12U-12U-17U
Inj: Oseltamavir 75mg BD
Inj: CLEXANE 40mg s/c o/d
Syp: CREMAFFIN PLUS (10 ml - 10ml)
BP, PR,SpO2 monitoring
Betadine mouth gargles- dilution with water
GRBS monitoring second hourly
15/05/2021
Head end elevation
O2 inhalation to maintain- If SpO2 > 90%
Tab: Dolo 650 mg/po/sos
Tab: MUT OD
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
IVF: 2ONS @75ml per hour
Inj: HAT 6ml 12U-12U-12U
Inj: Oseltamavir 75mg BD
Inj: CLEXANE 40mg s/c o/d
Syp: CREMAFFIN PLUS (10 ml - 10 ml)
BP, PR,SpO2 monitoring
Betadine mouth gargles- dilution with water 4 to 5 times a day
GRBS monitoring second hourly
16/05/2021
Head end elevation. O2 inhalation to maintain- If SpO2 > 90%
Tab: Dolo 650 mg/po/sos
Tab: MUT OD
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
IVF: 2ONS @75ml per hour
Inj: HAT 6ml 16U-16U-16U
Inj: Oseltamavir 75mg BD
Syp: CREMAFFIN PLUS (10 ml - 10 ml)
BP, PR,SpO2 monitoring
Betadine mouth gargles- dilution with water 4 to 5 times a day
GRBS monitoring second hourly
T Dexamethasone 4mg /BD
Prone position
17/05/2021
Inj 8am: NPH-10units,HAI 8 units
1pm: HAI:8 units
8 pm: NPH:8 units ,HAI 8unit O2 inhalation to maintain- If SpO2 >92%
Tab: pcm 65mg/ sos
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
Tab dexamethasone 4 mg /po/bd
Betadine mouth gargling
Inj.PANTOP40mg/iv/OD
Monitor vitals
18/05/2021
O2 inhalation to maintain- If SpO2 >90%
Tab: Dolo 650 mg/po/sos
Tab pan 40 mg/po/od
Tab: MUT OD
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
T Dexamethasone 4mg/po/BD
IVF: 2ONS @75ml per hour
GRBS:charting 8th hourly
INJ HAI
8AM ;NPH 10U,HAI 8U
1pm: HAI 8U
8 PM : NPH 10U ,HAI 8U
Glimipiride1 mg po/OD
19/05/2021
O2 inhalation to maintain- If. SpO2 >90%
Tab: Dolo 650 mg/po/sos
Tab pan 40 mg/po/od
Tab: MUT OD
Tab: Limcee/po/OD
Nebulization/Duolin & BUDECORT 8th hourly
T Dexamethasone 4mg/po/BD
IVF: 2ONS @75ml per hour
GRBS:charting 8th hourly
INJ HAI
8AM ;NPH 10U,HAI 8U
1pm: HAI 8U
8 PM : NPH 10U ,HAI 8U
T Glimipiride1mg/po/OD
Monitor SpO2,PR,BP,TEMP
Inform sos
T.Glimipiride0.5 mg po/ODS
FOR DIABETES
T.Glimiperide 1mg PO/OD / MORNING
T.Glimepiride 0,5 mg PO/OD/NIGHT
T.Metformin 500mgPO/BD/( 1-x-1)
ADVICE AT DISCHARGE
OXYGEN INHALATION TO MAINTAIN SpO2 >90%















Comments
Post a Comment